Berberine, AMPK, and Metformin
So, berberine, Metformin, and AMPK.
Berberine is a pretty interesting supplement. It’s been used for thousands of years in traditional Chinese medicine, and can be a useful adjunct therapy for quite a number of chronic conditions; from high blood pressure to diabetesand hyperlipidemia to cancer and so on. The fact that it has uses for all of these conditions that are all closely related with minimal to no side effects makes berberine a very interesting compound to study. To put the cherry on the cake, it’s also pretty cheap.
How does berberine work?
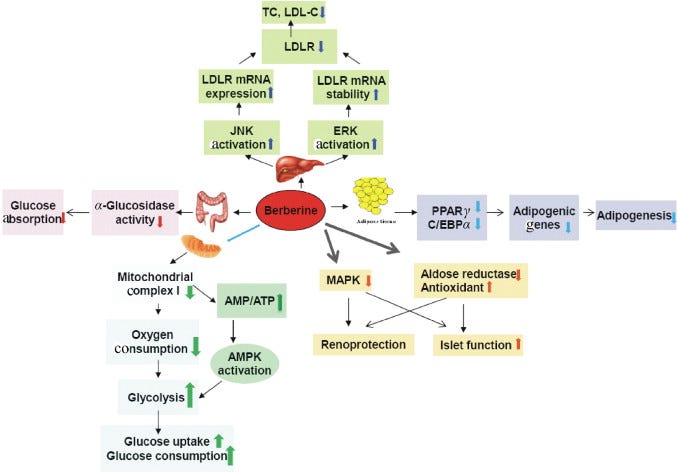
Well, there are a number of mechanisms that are involved in the benefits of berberine. The anti-hypertensive effects seem to come from the increased bioavailability of Nitric Oxide and a inhibition of ACE, resulting in increased ability to vasodilate and reduced pressure on blood vessels. As summarized by Yin et al. in 2012 (see image above), the reduction in LDL induced by berberine is caused by an increase in LDL receptors, and thus a higher metabolism of LDL.
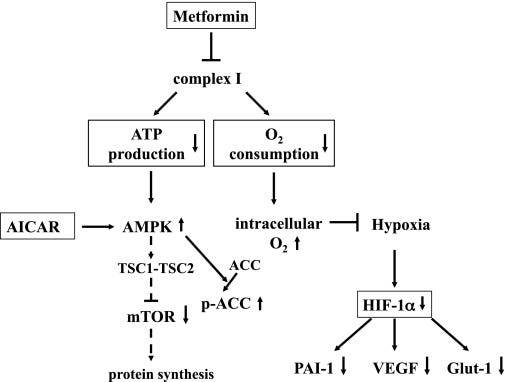
But diabetes is probably the most interesting and relevant condition for berberine supplementation. Berberine seems to improve glucose tolerance by the inhibition of mitochondrial complex 1 of the respiratory chain, which reduces the membrane potential of the inter-membrane space causing reduced efficiency in the production of ATP. The resulting decrease in cellular ATP then causes an increase in AMP and ADP, which then activates AMP Kinase (AMPK; more on this later). This then results in improved ability to pull glucose from the blood and into the tissue, a very desirable effect.
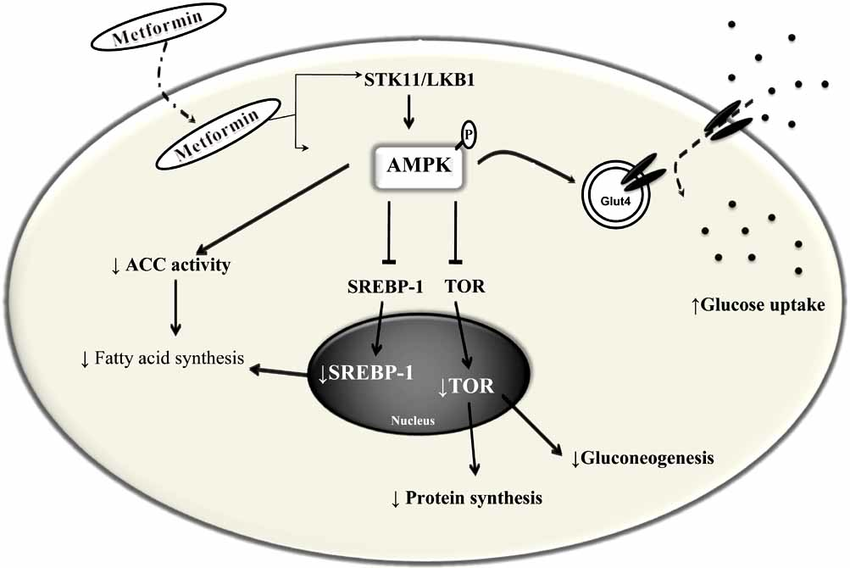
Even more interesting, and the last part of my title, is that Metformin and berberine appear to act upon the same pathways to improve insulin sensitivity.
So what’s with AMPK?
I think it’s appropriate to think of AMPK as an enzyme that senses low energy levels (more specifically, ATP) and activates numerous pathways to restore the intracellular ATP. Activation of AMPK usually increases glucose metabolism and the ability to pull glucose into the cell via GLUT4.
Pretty nice, huh? Metformin/Berberine → low ATP → high AMP/ADP → activation of AMPK → increased glucose transport into cells and glucose metabolism.
But I think these mechanisms beg the question: what are the implications of inhibition of complex 1?
In short, I’m not sure we completely understand, but I can take a solid stab at it. Here’s my thinking:
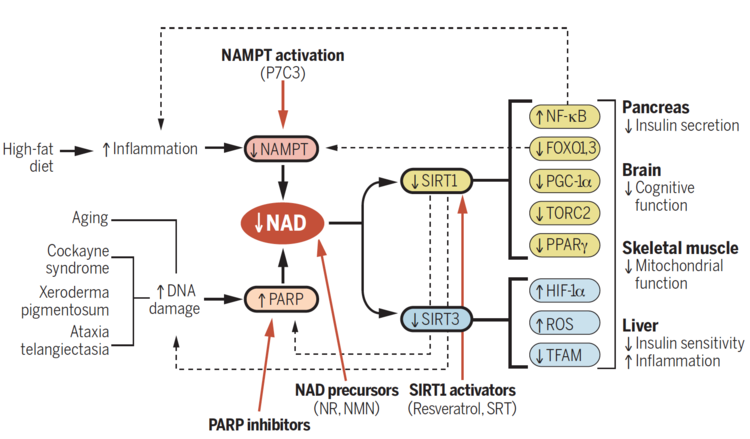
Complex 1 is also known as NADH dehydrogenase and is involved in the oxidation of NADH to produce NAD+. If complex 1 becomes inhibited, I think it is very clear that there is the potential to run the risk of a buildup of NADH, and a lack in levels of NAD+. In fact, low NAD+ and high NADH have already been proposed to be an issue in diabetes (therefore, I think I’m hitting the nail on the head up to this point). Nice, but so what?
Lower levels of NAD+ may be an important contributor to further progression of diabetes. I think that by using complex 1 inhibiting compounds, we may actually be exacerbating the metabolic effects associated with diabetes and other metabolism-related disorders, and impacting mitochondrial function and overall metabolic efficiency. Low NAD+ decreases the signaling for mitochondrial biogenesis and function, and may prevent scavenging of ROS. This, in turn, would further decrease insulin sensitivity and metabolic function, leading to further decrements in physical capacity and quality of life in these already sick individuals.
Of course, I think this all may depend on the #context, and the chicken or the egg argument. It hasn’t been decided if low NAD+ is caused by diabetes treatment (i.e. metformin, since it is a common first-line therapy), or the condition itself, or even obesity and chronic overnutrition. And, lastly, does berberine have the same effects as metformin, due to berberine’s activation of FGF-21?
No comments:
Post a Comment