Absorb More Nutrients with Digestive Enzymes
The phrase ‘you are what you eat’ is a fallacy. The truth is you are what you digest — and digestive enzymes are key to both better digestion and nutrient absorption.
Surprising as it may seem, up until relatively recently, little was known about how your digestive system actually works. Today, there’s a growing incidence of illnesses that, when traced back to the source, appear to be linked to nutrient malabsorption due to a lack of digestive enzymes. (1)
The Chinese proverb, “He that takes medicine and neglects diet, wastes the skill of the physician,” may not quite be as true as we like to believe. Oftentimes, good nutrition on its own isn’t the only issue involved in maintaining good health and avoiding illness.
What Are Digestive Enzymes?
The role of digestive enzymes is primarily to act as catalysts in speeding up specific, life-preserving chemical reactions in the body. Essentially, they help break down larger molecules into more easily absorbed particles that the body can use to survive — needless to say, an important role in digestive health!
The duodenum (the first and shortest segment of the small intestine) is a busy place: amino acids are extracted from proteins, fatty acids and cholesterol from fats, and simple sugars from carbohydrates. Nuclease cleaves (or splits) the nucleic acids essential for DNA into nucleotides. All the macronutrients are broken down into molecules small enough to be carried in the bloodstream and boost metabolism to ensure it runs effectively. Micronutrients, if they haven’t already been cleaved in the stomach acid, are released and transported into the bloodstream, too.
The pancreas produces bile salts or acids — which comprise water, electrolytes, amino acids, cholesterol, fats and bilirubin — and these are all sourced from the liver via the gallbladder. It’s the cholic and chenodeoxycholic acids that, when combined with the amino acids glycine or taurine, produce the bile salts themselves. The bile salts break down fats in food to enable the lipase enzyme to reduce further. (2)
In regard to mostly sugar metabolism, intestinal enzymes include the following key (but complicated!) processes: (3)
- Aminopeptidases degrade peptides into amino acids.
- Lactase, a dairy sugar, converts lactose to glucose.
- Cholecystokinin aids digestion of proteins and fats.
- Secretin, as a hormone controls, the secretion of the duodenum.
- Sucrase converts sucrose to disaccharides and monosaccharides.
- Maltase converts maltose to glucose.
- Isomaltase converts isomaltose.
Dealing primarily with fats and amino acids, pancreatic enzymes include: (4)
- Lipase converts triglycerides into both fatty acids and glycerol.
- Amylase converts carbohydrates into simple sugars.
- Elastases degrades the protein elastin.
- Trypsin converts proteins to amino acids.
- Chymotrypsin converts proteins to amino acids.
- Nucleases convert nucleic acids to nucleotides and nucleosides.
- Phospholipase converts phospholipids into fatty acids.
Digestive enzymes aren’t just beneficial, they’re essential! They break down food into amino acids, fatty acids, cholesterol (yes, it’s important to have cholesterol), simple sugars and nucleic acids, which help make DNA.
A six-step process, starting with chewing, triggers a domino effect in firing off mechanisms and secretions:
- Salivary amylase released in the mouth is the first digestive enzyme to assist in breaking down food into its component molecules, and that process continues after food enters the stomach.
- The parietal cells of the stomach are then triggered into releasing acids, pepsin and other enzymes, including gastric amylase, and the process of degrading the partially digested food into chyme (a semifluid mass of partly digested food) begins.
- The acid also has the effect of neutralizing the salivary amylase, allowing gastric amylase to take over.
- After an hour or so, the chyme is propelled into the duodenum (upper small intestine), where the acidity acquired in the stomach triggers the release of the hormone secretin.
- That, in turn, notifies the pancreas to release hormones, bicarbonate, bile and numerous pancreatic enzymes, of which the most relevant are lipase, trypsin, amylase and nuclease.
- The bicarbonate changes the acidity of the chyme from acid to alkaline, which has the effect of not only allowing the enzymes to degrade food, but also bacteria not capable of surviving in the acid environment of the stomach to break it down further.
At this point, for people without digestive enzyme insufficiency, most of the work is done. For others, supplementation is needed and helps this process along.
Who Should Take Digestive Enzymes?
Depending on how you view nutrition today, you either take a proactive or reactive approach to digestive enzyme supplements. On one side of the coin, “if it ain’t broke, don’t fix it, right?” This perspective holds that, unless someone has digestion concerns, taking enzymes is simply not needed. On the other side, with the depleting nutrient supply in our diets and influx of chronic disease, a little extra help couldn’t hurt.
Either way you look at it, an increasing number of people take digestive enzymes today, and certain health conditions like the ones below are good reasons to supplement.
Digestive Diseases
If you have any type of digestive disease such as acid reflux, gas, bloating, leaky gut, irritable bowel syndrome (IBS), Crohn’s disease, ulcerative colitis, diverticulitis, malabsorption, diarrhea or constipation, then digestive enzymes can help. Digestive enzymes can take stress off of the stomach, pancreas, liver, gallbladder and small intestine by helping break down difficult-to-digest proteins, starches and fats.
Age-Related Enzyme Insufficiency
As we age, the acidity of our stomach acid becomes more alkaline. In respect of enzyme production, this means there’s an increasing likelihood the acidic “trigger” produced when chyme enters the intestine may fail. If the acidity trigger fails, then the “signal” isn’t given to secretin, which in turn prevents pancreatic secretions from releasing.
Concurrent illnesses aside, as we age there’s increasing suspicion that digestive problems may result from either low stomach acid or enzyme insufficiency in the elderly, which could be what causes acid reflux. (5)
Hypochlorhydria
It’s not only the elderly who suffer from hypochlorhydria or have too little stomach acid. (6) Aside from a decrease in stomach acid that fails to trigger reactions, the acid itself cannot break down foods to release minerals, vitamins and nutrients. Many micronutrients are “cleaved” or released from food while it’s in the stomach — if this action fails, then there’s an automatic nutritional or enzymatic insufficiency.
Liver Disease
Anyone with liver disease should be suspected as having a concurrent enzyme insufficiency. One of the more common conditions is known as alpha-1 antitrypsin deficiency, a genetic disorder that affects roughly one in 1,500 people worldwide. (7) Typically first hitting adults between ages 20–50 with breathing and other respiratory complaints, as roughly 15 percent of adults develop liver disease.
Other illnesses, which may at first diagnosis appear unrelated to enzymatic deficiency, also deserve attention:
- Crohn’s disease may result in enzyme deficiency.
- Iron deficiency or vitamin B12 deficiency may suggest that the digestive process is failing to cleave these nutrients from food.
- Vitamin D deficiency may indicate another malabsorption issue, just like night blindness can result from a vitamin A deficiency.
Diagnosed illnesses aside, there are many symptomatic indicators of enzymatic insufficiency. Although some could be attributed to other conditions, several relate primarily to the failure of pancreatic enzymes to be released.
- Stool changes — If the stool is pale and floats in the toilet bowl, because fat floats, this is indicative of pancreatic enzymes not functioning correctly. Another indication can be greasy or fatty deposits left in the toilet water after you poop.
- Gastrointestinal complaints — Another indicator, together with stomach distention, around an hour after eating is diarrhea. Flatulence and indigestion are also indicative that the patient may have an enzyme insufficiency.
- Fluoridated water — Further, recent research suggests that fluoride in water may be responsible for the decreased activity of both pancreatic lipase and protease. (8) The study, although carried out on pigs, has broad-ranging implications relative to increased free radical damage and loss of mitochondria production.
The answer to the increasingly asked question — “Who should take digestive enzymes?” — may ultimately turn out to be many more people than first envisaged!
Digestive Enzyme Benefits
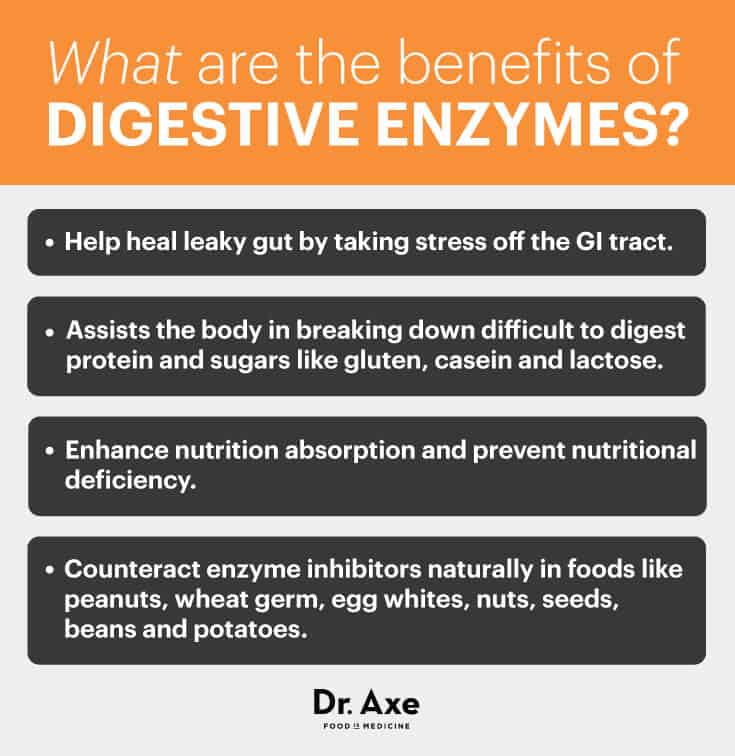
What are the benefits of digestive enzymes?
The answer is simple: Without them, we couldn’t process food! With that said, there are three main reasons why most people should take digestive enzymes:
- Help heal leaky gut by taking stress off the GI tract.
- Assists the body in breaking down difficult-to-digest protein and sugars like gluten, casein and lactose.
- Greatly improve symptoms of acid reflux and IBS.
- Enhance nutrition absorption and prevent nutritional deficiency.
- Counteract enzyme inhibitors naturally in foods like peanuts, wheat germ, egg whites, nuts, seeds, beans and potatoes.
What Are the Best Digestive Enzyme Supplements?
Digestive enzyme products are derived from three sources:
- Fruit-sourced — usually pineapple– or papaya-based.
- Animal-sourced — including pancreatin sourced from ox or hog.
- Plant-sourced — from probiotics, yeast and fungi.
Vegetarian Products
Products in the digestive enzyme range can present a dizzying array of ingredients. Some contain only plant-based enzymes, which are aimed at vegetarians and vegans. These usually at least contain the health benefits of bromelain, an enzyme derived from the pineapple, and many more include papain enzyme from the papaya.
In addition, some have complementary herbs and spices. Amla (gooseberry) extract — which isn’t an enzyme but a herbal remedy from Ayurveda medicine taken for general well-being — is often included. It’s believed to work in synergy with the other compounds.
Products designed specifically for vegans are available. In most cases, the pancreatin source in these products are, as with lipase, derived from Aspergillus niger. This is a fungus-based, fermented product rather than ox or hog bile, which is the usual extract.
Full-Spectrum Digestive Enzymes
Be sure to look for a full-spectrum enzyme blend for general digestive improvement. Here are some tips:
- If you have gallbladder issues and are looking for a gallbladder diet natural treatment, purchase one with more lipase and bile salts.
- Where you see betaine HCL listed as a product ingredient, make sure pepsin is also included.
- Others contain lactase, which until recently was only available as an individual product. This enzyme is designed to assist those with specific issues relating to sugar absorption from dairy products.
- Choose a blend with herbs, such as peppermint and ginger, that support digestion.
- Also, because some people need more pancreatic enzymes than others, you need to bear in mind the level of each dependent on your needs. (9) Most products contain some level of pancreatin, which is a combination of all three pancreatic enzymes.
At the end of the day, there is no doubt that many people benefit from taking enzyme supplements.

No comments:
Post a Comment